「Doctor Isao Koshima and Devices Supporting Transcending Techniques」
Our item was introduced as "The needles and thread that are essential for the surgery performed by Dr. Koshima are manufactured by Kono Seisakusho"
↓↓ The following is the full article ↓↓
[PAGE 1]
Doctor Isao Koshima and Devices Supporting Transcending Techniques - A World-leading Plastic Surgeon who is Rebuilding Patients' Lives
"A Living Legend - A Lifetime Review of His IKIZAMA - Last Live Show"
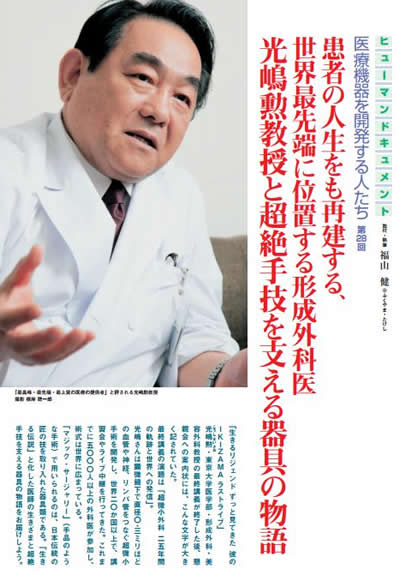
This is what it said in large letters on the invitation to the gathering held after Doctor Isao Koshima, a professor at the Department of Plastic, Reconstructive & Aesthetic Surgery, University of Tokyo Hospital, completed his final lecture.
The title of his final lecture was "Ultra Microsurgery - Trajectory Over 25 Years and Transmission to the World".
Dr. Koshima developed ultra microsurgery, which involves linking blood vessels, nerves and lymph nodes of 0.3 mm in diameter with microscopic guidance. He has held lectures on and live relays of actual ultra microsurgery in over 20 countries worldwide. He has been involved in the surgery of over 5000 patients and his surgical techniques are spreading globally.
Devices incorporating traditional Japanese craftsman techniques are used in "magic surgery". We will examine the way of life of a doctor who became a living legend and the devices supporting transcending techniques.
[PAGE 2]
A Surgical Technique from Japan that became a World Standard
"I never dreamed that a day would come when I, who was shedding tears of misery every day, would shed tears of joy. The surgery that you performed on me changed my life from one of despair to one of hope. I think that reconstructive plastic surgery also reconstructs peoples' lives."
Doctor Isao Koshima, a professor at the Department of Plastic, Reconstructive & Aesthetic Surgery, University of Tokyo Hospital who receives letters such as these, held his final lecture on March 10, 2017 at the University of Tokyo Experimental Research Building Iron Gate Commemorative Auditorium.
The title was "Ultra Microsurgery - Trajectory Over 25 Years and Transmission to the World".
Ultra microsurgery requires the skills to connect blood vessels etc. of 1 mm or smaller with microscopic guidance. Joining disconnected blood vessels and nerves is referred to as anastomosis. In reconstructive surgery, the smaller the anastomosed blood vessels and nerves, the smaller the physical burden on the patient and the greater the satisfaction of the patient.
Of the difficult techniques involved in reconstructive surgery, anastomosing microscopic blood vessels with diameters of 1 mm or less requires that the surgeon learn extremely difficult techniques. Dr. Koshima is an expert even in this field of specialized reconstructive surgeons. Using a microscope and a specialized 0.05 mm needle, he pioneered a technique for anastomosing 0.3 mm blood vessels and nerves to create a new surgical procedure. He is truly a leader amongst trailblazing doctors worldwide.
During his final lecture, photographs of Dr. Koshima in his days at the Tottori University Faculty of Medicine engaging in judo and wearing a hakama (traditional Japanese men's suit) with a katana sword were displayed. As the captain of the judo club, he was strong enough to fight the campaign of the riot police group of the local police force. He also became immersed in iaido (art of drawing the Japanese sword) in which the winner of the match is determined the moment the sword is drawn from its sheath, becoming a grade holder in the sport. As a young doctor who enjoyed martial arts, he directly decided to start on the path of plastic surgery after discovering in university lectures that this field of surgery could erase the ugly scars that he had. Over the following 25 years, this surgical field evolved from microsurgery to super microsurgery and then to ultra-microsurgery, which is currently available.
The homepage of the Department of Plastic, Reconstructive & Aesthetic Surgery, University of Tokyo Hospital displays a photograph of Dr. Koshima, a 4th generation professor, together with the following description of his fields of strength.
"I specialize in the partial restorative surgery of lost body parts and reconstructive medicine using autologous tissue. I also specialize in cosmetic and reconstructive surgery of post-cancer resection head and neck parts, the upper and lower neck, face, limbs and breasts etc., hand surgery, lower limb surgery, functional reconstructive surgery for lymphedema and neuroparalysis of the facial nerves and limbs, treatment of congenital defects in the skull, face or hands and feet (cleft lip and cleft palate, microtia, skull and facial bone abnormalities, facial fat atrophy, finger defects etc.) and angioma (arteriovenous malformations), treatment of lower limb osteomyelitis, refractory ulceration, post-cosmetic surgery complications (foreign material infection in breast/s, neuroparalysis etc.), restoration of lost fingernails/toenails, and the treatment of lymphedema, bedsores, refractory ulceration, osteomyelitis, diabetic ulcers, and various tumors (parotid gland tumors, skin cancer, soft tissue sarcomas)."
What Dr. Koshima pioneered in the areas of partial restorative surgery of lost body parts and reconstructive medicine using autologous tissue, which he mentions in this self-introduction, is reconstructive surgery using perforator flaps. Since this technique was developed in Japan in the 1980s, various reports of successful cases at international workshops held each year and awareness-raising activities have resulted in it becoming the first choice for surgery in the field of reconstructive surgery, and it is also recognized as a technique that needs to be standardized.
[PAGE 3]
Unbelievable - It's a Trick
What does reconstructive surgery using perforator flaps involve?
"Perforators" and "flaps" are not words that are commonly used.
A perforator refers to a thin blood vessel that runs toward fat layers or skin after branching off from a thick blood vessel running through or under a muscle. A flap refers to a piece of skin with blood flow.
Even if people are not completely familiar with the pronunciation or meaning of the terms involved, perforator flaps have spread in popularity as a result of overwhelming support from people who require the reconstruction of some part of their body.
A typical example of this is women requesting breast reconstruction after undergoing mastectomy to treat breast cancer.
According to Dr. Koshima, before perforator flaps were developed, muscle flap surgery was used. This involved adding fat and muscle to the skin of the rectus abdominus muscle of the lower abdominal region or the latissimus dorsi muscle, which expands from the back to near the lower back before collecting the muscle for transplantation. Breast reconstruction requires relatively large and soft tissue. Although such tissue is often collected from the abdominal region, this can weaken the abdominal muscles as muscular tissue is also collected in the process. As a result, it wasn't uncommon for patients to suffer from abdominal pain or hernia postoperatively. In cases in which a latissimus dorsi muscle flap is transplanted to the chest, some patients also experience movement of the transplanted back muscle when they move their scapula.
However, by connecting perforators, which are very small blood vessels of 0.5 mm in diameter that transport oxygen and nutrients to fat tissue, Dr. Koshima has proven that fat tissue can be fully engrafted with perforator flap surgery that does not cause any damage to the abdominal muscles. This went against the common mindset of plastic surgery at the time, which dictated that engraftment of tissue was unlikely unless blood vessels running through muscle tissue were connected. As a result, his methods received little understanding not only within Japan, but also overseas.
Dr. Koshima states, "I developed perforator flap surgery in 1986. I then developed a method of breast reconstruction preserving the abdominal muscles in 1989. Nobody believed me. In 1989, I sent a manuscript to the most renowned plastic surgery journal in the US. However, after waiting for 1 year, my manuscript was rejected and even ridiculed, with the comment, 'It's impossible - It must be a trick.' Despite this, perhaps one editor felt that maybe it was true. They told me to try submitting my manuscript to a UK journal. After sending it to the said UK journal I waited another year, after which I received notification that it would be published."
In 1990, Dr. Koshima again performed a method of surgery that would attract attention from plastic surgeons around the world.
[PAGE 4]
This was lymphaticovenular anastomosis, which involves connecting lymph ducts with veins to return lymphatic fluid and cure edema.
Dr. Koshima states, "Now, in 2009, there are said to be 100,000 to 150,000 lymphedema patients throughout Japan. When cases from overseas are also included, this indicates that an unfathomable number of patients are suffering without even being able to receive psychotherapy.
Lymphedema treatment involves physiotherapy focusing on compression therapy. Surgical treatment for this condition has been consistently rejected. Having to wear sleeve stockings every day to prevent the exacerbation of edema places a significant physical and psychological burden on patients. Therefore, patients have long desired to undergo surgical treatment, which could relieve them of both the edema itself and the required physiotherapy. Despite this, surgeons have been unable to completely respond to these needs."
In the preface of "All About Lymphedema - From Anatomy and Physiology to Conservative Treatment and Surgical Therapy" (2011, Nagai Shoten), which Dr. Koshima edited, he writes as follows:
The Three Types of Lymphangiosarcoma Cancer disappeared
Lymphedema refers to a state of swelling (edema) of the arms and legs resulting from a buildup of lymphatic fluid in the muscle and fat tissue due to blockage of the lymph ducts, which transport metabolic waste products.
Moreover, 80% to 90% of these cases result from resecting the lymph nodes, which act as filters for cancer cells, during surgery for diseases such as uterine cancer or breast cancer or the application of radiation resulting in decreased lymph duct function. Some cases occur soon after surgery, whereas other cases occur 5 or even 10 years later. If the condition develops in the patient's arms and symptoms progress, the patient will find it difficult to hold and grasp things. They will eventually become unable to write, hold a knife or chopsticks. If it occurs in their legs, it will become difficult to walk, they will become unable to go outside or even move about indoors, placing limitations on their range of activities and behavior. Many patients also suffer from psychological distress over changes to their physical appearance. They stop wanting to go out or meet people, and lose motivation and can fall into a state of depression.
The statement in the preface of "...patients have long desired to undergo surgical treatment, which could relieve them of both the edema itself and the required physiotherapy. Despite this, surgeons have been unable to completely respond to these needs" is suggestive of Dr. Koshima's feelings of regret as a plastic surgeon. However, it also appears that this feeling appeared to be the passionate origin of his cultivation of the lymphaticovenular anastomosis procedure.
He said, "If I tell the patient that they can't be cured, they will lose all hope. I want to help patients in any way that I can. This has also become a motivating force behind my polishing of and technical improvements to various new adjustments to surgical procedures."
Lymphaticovenular anastomosis involves connecting 0.3 mm diameter lymph ducts to small 0.6 mm veins to allow the built up lymphatic fluid to flow into these veins, thereby relieving the edema.
Dr. Koshima found that when lymphaticovenular anastomosis was performed on arms in which lymphedema had developed, great improvement was seen. However, the anticipated effects were unable to be achieved in legs in which lymphedema had developed. To find out the reason for this, he sampled lymph duct tissue and observed the detailed mechanisms of lymph duct tissue with an electron microscope. As a result, he found that smooth muscle cells in the tunica media of major lymph ducts and lymph nodes returned lymphatic fluid by strongly contracting and undergoing sluggish pressure changes two to four times each minute.
Previously, it was thought that lymphatic fluid was transported by means of passive factors such as muscle and respiratory movement, and the beating of arteries. This is also why elastic clothing and physiotherapy such as massage came to be recommended.
When lymph nodes in the limbs are resected, peripheral lymph duct expansion and degeneration and disappearance of smooth muscle cells occurs within a short period of time. Even if the lymph duct has been connected to a vein, if the smooth muscle cells undergo degeneration and stop performing contraction, lymphatic fluid will be unable to flow. Therefore, Dr. Koshima developed a method of surgically creating a bypass through which lymphatic fluid could flow and compressing it with an elastic stocking in place of smooth muscles. This method resulted in a dramatic improvement in the healing rate.
He also hopes to improve the surgical procedure and discover a method for detecting the buildup of lymphatic fluid before the patient's legs became swollen with lymphedema. He will develop a method of preventing edema with anastomosis before the smooth muscle cells become degenerated and any functional impairment occurs in the smooth muscle cells. This could free people from suffering from lymphedema throughout their lives.
Currently, the field of plastic surgery plays a vital role in treatment for lymphedema. In this sense, it appears that the desires of patients "to undergo surgical treatment, which could relieve them of both the edema itself and the required physiotherapy" have been answered.
An even more sensational result has been born from lymphaticovenous anastomosis. This is the fact that sarcomas in lymph ducts and blood vessels that occur in 0.4% of edema patients might be able to be cured with lymphaticovenous anastomosis. Lymphangiosarcomas are a malignant type of tumor and the 5-year survival rate is not very high.
If a patient is diagnosed with a lymphangiosarcoma at a department of plastic surgery, they are referred to a department of dermatology and treated with anticancer drugs. One such patient reported that their cancer disappeared. While this was considered to be a result of the anticancer agents, another patient reported that their cancer also disappeared in 3 months.
Investigation of what these two patients had in common revealed that they had both previously undergone lymph duct bypass surgery.
[PAGE 5]
Just as he was conjecturing, "Perhaps anastomosing lymph ducts suppresses the cancer itself but anti-cancer immunity arising after cancer actually killed the cancer cells," a patient who had developed a sarcoma and had not undergone any treatment visited Dr. Koshima with a referral from a compression therapy doctor.
He immediately performed a biopsy to determine whether it was an angiosarcoma and decided to perform bypass surgery on the foot instep on one side only.
"The three types of cancer that were present all disappeared. The cancer was defeated and collapsed in on itself. I became convinced that this method was unquestionably effective. I thought that if there had been similar cases in the past, they would already have been reported and investigated whether there were any such cases. As a result, I found that the cancer had also disappeared in two such cases.
In fact, these cases were reported by a dermatologist who I knew from when I was at my previous assignment, at Okayama University. When I investigated this in more detail, I found that I had performed the lymph duct bypass surgery on one of the two cases. The other case had undergone surgery performed by a doctor who had been overseen by a former pupil of mine after I came to the University of Tokyo. The cancer had truly disappeared.
This meant that there were three such cases. Of the 12 sarcoma cases that I had been involved in treating, when the two cases mentioned at the beginning were added, this meant that there were five cases in which the cancer had disappeared, and all of these patients were living. This is remarkable considering that the survival rate for sarcoma is 5 to 8%. One patient has even survived for 8 years. Although I haven't released this in a report, it has come to be recognized worldwide that this fact truly appears to have been proven."
The Motivation for Development was "Eliminating Doctorless Villages"
After being awarded a bouquet of flowers at his final lecture, professors from other treating departments commented on Dr. Koshima. One notable comment was that by a professor who said of watching Dr. Koshima's surgical procedure, "I was simply amazed."
Since Dr. Koshima held his first workshop for perforator flap surgery in 1997 at Ghent University in Belgium with an audience of approximately 200 people, he has performed live surgery overseas in over 20 countries in order to popularize the new surgical procedure. As over 5000 surgeons have participated in such workshops, the procedure has spread throughout the world.
Doctors from America and Europe expressed admiration upon seeing Dr. Koshima's surgical technique, which involves separating a 0.3 mm blood vessel and sewing it to a 0.8 mm vein with six stitches. They praised it as "magic surgery" as it appeared to them that the surgery was being performed with a magic trick. Dr. Koshima practiced this procedure, which appears to be like some kind of magic, countless times in order to master it.
After entering the department of plastic surgery, he would become absorbed in suturing the blood vessels of mice using a surgical microscope from when he finished work until late into the night. Mouse blood vessels are delicate and weak. If your finger deviates just slightly, the thread becomes tangled and the blood vessel becomes blocked.
Over the course of many days observing and joining microvasculature under a microscope, he learnt that even nerves have a network of capillaries and that no matter how small the nerve, it had a network of feeding vessels. If these could be joined, there would be feeding vessels present from directly after surgery, making it possible for the transplanted nerve cells to survive. This is how he came up with the idea of mastering a technique of nerve grafting involving joining microvasculature so as to connect living blood vessels.
"This was when I was in my 20s, soon after I became a doctor. That makes it around 40 years ago. This is still my specialty. At the time, I received a lot of opposition... some people criticized the idea as being experimental surgery. However, it simply meant performing nerve grafting and connecting feeding vessels so it didn't involve any risks. When performing surgery on a girl who had lost a fingertip, I resected one of her toes and joined it to her finger. That was around 1990. When the microvasculature is connected, the success rate is close to 100%."
The East is said to be ahead of the West in the field of plastic surgery. This is because of the dexterous fingertip skills of people raised in cultures that use chopsticks.
Grasping grains of rice with chopsticks is not that difficult for people who have been raised in a culture of using chopsticks to eat from infancy. This is difficult for Westerners, who have been raised to eat meals with a knife and fork. While doctors in China and South Korea are just as dexterous in terms of fingertip skills, doctors in Japan remain overwhelmingly superior in the field of super microsurgery. What could be the reason for this? Apparently, it is related to the medical devices used in surgery.
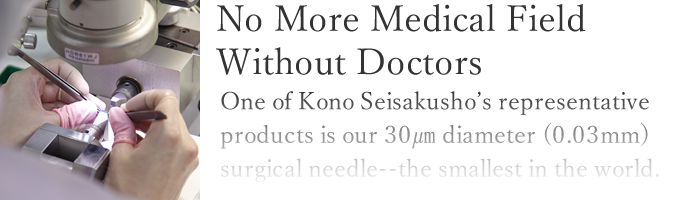
"My work involves separating and connecting blood vessels of up to 0.3 mm in size. In relative terms, one strand of hair is 0.1 mm, so that means that the blood vessels that I deal with are about as thick as three strands of hair. The needles used to suture such blood vessels are one tenth of that size. For 0.5 mm blood vessels, I would use a 0.05 mm (50 micron) needle. A 50 micron needle can hardly be seen with the naked eye. All of the devices such as needles, suture thread and needle holders that are essential for surgery are made in Japan. Precise machining technology unique to Japan is supporting world-leading surgical techniques."
The needles and thread that are essential for the surgery performed by Dr. Koshima are manufactured by Kono Seisakusho, the main factor of which is located in Ichikawa City, Chiba Prefecture, Japan.
Upon stating the destination to a taxi driver after arriving at JR Ichikawa Station, the taxi driver starts driving after saying, "Ah, that's the place that the Emperor of Japan came to see, isn't it?"
[PAGE 6]
Kono Seisakusho is a leading company in Chiba Prefecture that has also received many awards.
A list of just the major awards that the company has received includes the Chiba Prefecture Venture Business Operator Award/Excellent President Award, the Japan Society of Mechanical Engineers Kanto Branch/Technique Award, the 14th Chiba Genki Shirushi Corporate Awards/Award for an Excellent Product or Service, the 3rd Japanese Award for Manufacturing/Prime Minister's Award, the Japan Creation Awards 2010/Micromedical Award and the 20th Chiba Genki Shirushi Corporate Awards/Chiba Prefectural Governor Award.
President Junichi Kono says that the aim of the company in engaging in the challenge of developing the world's smallest needle, with a diameter of 0.03 mm was "eliminating doctorless villages."
"At the time, it was commonly believed that it was impossible to manufacture needles smaller than 0.1 mm. The surgery field requiring needles smaller than 0.1 mm appeared to be like a doctorless village, or a blank area where no medical care was offered.
However, as there are people who require medical treatment even in doctorless villages in isolated areas, there are people who require surgery using a needle that is smaller than 0.1 mm.
[PAGE 7]
For example, if the finger of a young child were to be severed due to an accident of some sort, conventional surgical suture needles could not be used to reconnect it. If the microvascular could be operated on, it could offer hope to people with diseases that were previously considered difficult to treat. Even if the number of cases is small, there are people who are suffering in a blank area of medical care.
When a plastic surgeon who is a close friend of mine strongly urged me to develop a needle that could be used to perform surgery on tissue that was 0.5 mm or smaller, development was started with medical-engineering cooperation. While we did expect it to be fairly difficult to develop a product that significantly exceeded the common perceptions of that time, we decided to go ahead with the challenge. This was because we wanted to be the ones to create a surgical needle that could relieve situations of 'doctorless villages' in the field of microsurgery."
The Challenge of Developing a 0.03 mm Needle - the Smallest in the World
Although we were somewhat prepared for difficulties, we truly experienced the difficulty of newly creating something that does not yet exist.
While we had a wealth of experience in manufacturing surgical needles, conventional methods and knowledge were of no use in developing the 0.03 mm needle that Dr. Koshima wanted to use.
[PAGE 8]
This is what a process of repeated trial and error first led us to realize.
Tsutomu Iwadate, engineering corporate executive officer and head of the manufacturing technical department, was also involved in the development with Mr. Kono, He described the experience as follows.
"I was just absolutely focused on developing a needle that was so small that nobody else in the world had ever achieved such a feat. So when I faced difficulties, rather than being subjected to external pressure, I was actually the one placing pressure on myself.
Developing and manufacturing the smallest needle in the world required manufacturing equipment that could achieve extremely precise processing. However, at the time we did not have such precise production facilities. Naturally, as it was an untrodden region, there were no manufacturing equipment makers to which we could simply outsource operations. Therefore, we developed absolutely everything from the tools, to the manufacturing and testing equipment at our company. We truly started from square one.
We also found wiring processing difficult. The surgical needles used for microsurgery are used to penetrate vascular tissue. Therefore, they are like the ultimate knife. They must not only be thin, but also sharp and durable so that they do not bend when used for suturing. As requiring durability makes manufacturing more difficult, we found it very hard to strike an appropriate balance.
The suture thread used for microsurgery is characterized by the needle and thread being melded together. Previously, we connected these by using a laser to make an indentation in the end of the needle in the axis direction into which the thread was inserted. However, the small size of a 0.03 mm needle meant that the metal material itself would melt if a laser were applied, making things very difficult. Therefore, we developed a method of making a shallow split to the end of the needle like cracking bamboo, placed the thread between this and then fastened it back together to fixate it. Thus, we finally achieved the finished product 3 years after starting by first developing processing equipment to crack fine needles."
This development not only made it possible to perform surgery on tissue that was 0.5 mm or smaller in the field of plastic surgery, it also expanded the possible surgical field from microsurgery to super microsurgery and opened up possibilities for curing diseases that medicine has previously been unable to treat.
What both Mr. Kono and Mr. Iwadate emphasize is the fact that they also gained things during the difficult process of development.
Let us consider the main things that they gained.
★Analyzing the techniques of prominent persons and attempting to convert them to numeric terms.
Previously, fine processing technology for opening holes in needles to fixate suture thread was performed by one skillful craftsperson. However, he became ill and this skill was unable to be passed on. It was then that they truly realized the need to convert things into numeric terms. Since then, activities to convert advanced processing techniques into numeric terms have resulted in superfine needles that a craftsperson who had polished their skills over decades was able to produce with a success rate of approximately 10% can now be produced by general staff with a success rate of approximately 98%. Thus, the alternation of generations is now progressing well.
★Studying and utilizing traditional craft skills
The skills of a master traditional craftsperson have been utilized in the mechanism of the world's smallest surgical needle, with a diameter of 0.3 mm. Traditional craft skills have also been utilized in other products of the company, such as in the method of folding a fixation tape made of non-stretchy fibers and used for hernia treatment. There have also been many cases in the past where focusing on traditional craft skills has revealed the key to solving difficult problems. When developing a new product, traditional techniques that came about in Japan such as pottery, ironware and sword-making are studied and these techniques are passed on.
★Promoting medical-engineering cooperation to build a bridge between medicine and engineering
Seeds cultivated in the field of engineering can be connected to needs in medical settings. While this is the true ideal for medical-engineering cooperation, it is actually so difficult for smooth communication to be carried out between engineers and medical scientists that they often feel like they are speaking different languages.
[PAGE 9]
By becoming a bridge between these two fields, medical device developers enable the development of products with needs and seeds in a matched state. To technological development venture corporations, creating unique products through medical-engineering cooperation and constructing development systems for the small-lot production of a large variety of products is a great advantage.
Mr. Kono described his company's operating policy and principles, saying, "What we developed was the world's smallest needle. However, my job is to maximize what we gained along with that development and to utilize that throughout the organization."
"Our business model is manufacturing utilizing precise processing technology and it is based on the creation of new markets. We focus on niche areas that large corporations find it hard to respond to and develop and manufacture small-lot production of a large variety of products with high added value. We then develop this into highly profitable businesses. Our principle is to contribute to the development of medical technology and help as many patients as possible by responding to highly particular needs and through the new medical devices that we produce.